Is It Safe? Let’s talk about vaccines
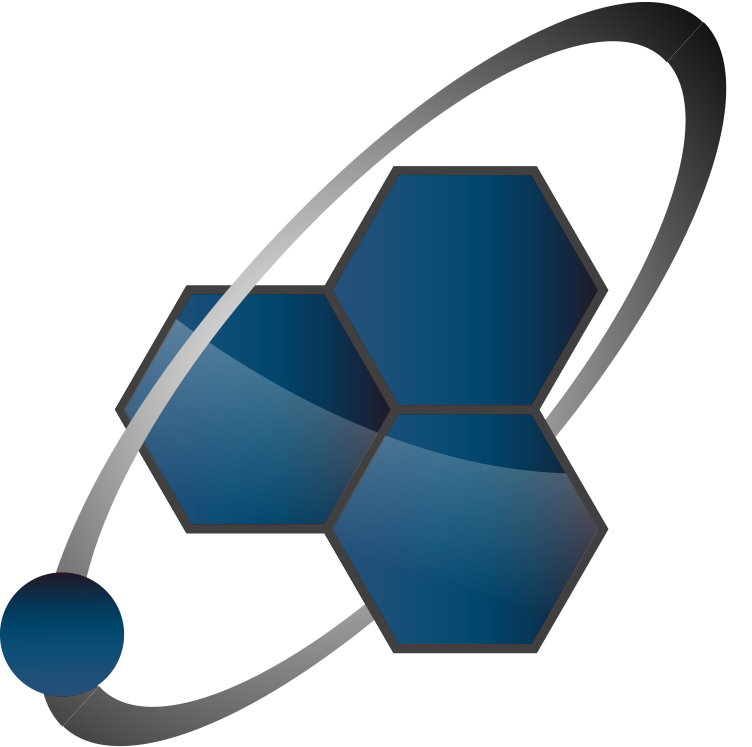
COVID vaccination record, image courtesy of Department of Defense/Operation Warp Speed
J&J is on hold. Are COVID vaccines safe?
Some years ago I discovered a website that “provides an unbiased data clearinghouse” on the controversy and dangers surrounding dihydrogen monoxide, or DHMO. According to the site, DHMO “is colorless, odorless, tasteless, and kills uncounted thousands of people every year…DHMO may cause severe burns; accelerates corrosion; is a major component of acid rain; and is found in biopsies of pre-cancerous tumors.” Nevertheless, DHMO is widely used as an industrial solvent, in nuclear power plants, in community swimming pools to maintain chemical balance; and also as an additive to many food products including jarred baby food, cough syrups, and beer.
At this point readers who have studied the nomenclature of organic chemistry will be chuckling. Di-Hydrogen (two hydrogen atoms) Mon-Oxide (one oxygen atom) = H2 O = H2O.
The dangerous chemical substance with the scary name is water. And every word about its risks is true on this website, which is a spoof of alarmist, conspiratorial, absolutist thinking.
I mention this parody to highlight a fundamental point about “safety.” Water is not “safe.” And if you think of “safety” as an on/off switch rather than a dial with settings between zero and a million, then nothing in this world is safe.
So when people ask me, are the COVID vaccines safe?, I first consider what they mean by “safe.” In most cases, they’re really asking, should I be vaccinated?
These are different questions.
Does that sound alarmist, or anti-vaxx? It shouldn’t. Consider these analogies.
- Is it safe to travel by car?
- Is it safe to take penicillin?
- Is it safe to have elective surgery?
If “safe” means there is zero risk of any bad outcome linked to the activity, then the answer is no. But if the question really is, should I get in a car, or take an antibiotic, or have my knee replaced, the answer is, it depends. It depends on the amount of risk and the amount of benefit in a quantitative sense. The question is not, is X safe? The question is, does the benefit of X outweigh the risk?
In the case of automobile travel, about one American dies for every 100 million vehicle miles traveled each year (source). In 2019 that added up to 36,120 fatalities. That doesn’t sound safe to me. If I derived no benefit from traveling by car, I would reject car travel. Yet I get in my car every single day. Like most Americans, I have decided that the benefits of vehicle travel greatly outweigh the risks.
Penicillin is an antibiotic drug used to treat bacterial infections. Since Florey & Chase figured out how to manufacture this miracle cure in the early 1940s, penicillin has probably saved the lives of a hundred million people or more. At the same time, however, about 1 in every 10,000 people who take penicillin experience anaphylaxis (source, source), a sudden and severe allergic reaction that can be fatal if untreated. Should you take penicillin, then? Only if the benefit to you is greater than the risk. If you have pneumonia or a wound infection, the answer is absolutely yes.
What about surgery? According to one study of a typical Western hospital over a twelve-year period, the mortality rate following elective surgery was 0.17% (around 2 deaths for every 1200 surgical procedures). Should you refuse all surgical procedures? Well, that depends on how much you have to gain from undergoing an operation.
Without even thinking about it, we apply this risk/benefit calculation to all kinds of choices in our daily lives. Am I going to drink a cocktail? Go downhill skiing? Get pregnant? None of these is “safe.”
What about vaccine safety?
In many of the examples I just gave, you can’t put a number on both the risk and benefit. I can tell you how many women die in childbirth, but I can’t quantify the benefit of being a mother. We can measure the number of ski injuries, but not the value of exhilaration on the slopes.
In that context, vaccines are easier to justify. We can approximately quantify the risk of contracting an infectious disease, and the chances of death or other serious outcomes from the infection. With proper study we can also quantify the protective benefit and the risk of adverse effects from the vaccine itself. Only by comparing these two can we answer the question, should we use this vaccine?
In the US, we have professionals whose job it is to do the math for us. Government officials (generally at the FDA) examine the available data on vaccine efficacy and safety, and decide whether the relative risk/benefit justifies use of that vaccine. To date, three vaccines against COVID-19 have met the standard for emergency use in the US. These approvals were based on data from clinical trials that looked for any safety problems in tens of thousands of people over months of time. Both the new mRNA-based vaccines (Pfizer and Moderna) and the new adenovirus-based vaccine (Johnson & Johnson) passed with flying colors: highly effective; no common or short-term safety problems.
But what if a vaccine has a rare adverse effect? Let’s say a vaccine causes a weird clotting disorder in one out of a million people. One in a million is a pretty rare event. That’s less likely than being struck by lightning (about 1 in 500,000 in the US per year), and far less likely than getting a severe case of COVID in 2021. Would such a side effect be detected in a clinical trial of 50,000 patients? Probably not. You would only notice once the vaccine had been given to literally millions of people. Then a handful might turn up, and you’d have to re-evaluate.
The challenge, of course, is to figure out whether a rare effect is a coincidence, or a consequence of the vaccine. On Tuesday morning, US federal health regulators recommended a pause in the use of Johnson & Johnson’s single-dose COVID vaccine so they can work on that very question. 6,800,000 Americans have received the J&J vaccine. After receiving the J&J vaccine, 6 Americans developed an extremely rare disorder of blood clots in combination with low platelets. (This is similar to what’s happening in Europe with the AstraZeneca vaccine, which is also adenovirus-based). During the pause, regulators will try to discern if there’s a connection between this clotting disorder and the J&J vaccine; and if so, whether they can identify people who are more or less likely to be affected.
We know for absolute sure that even if the adenovirus-based vaccines can trigger this clotting disorder, the effect is rare.
So is a COVID vaccine safe?
Safe relative to what? The only meaningful form of this question is, is it safer to get a vaccine than to go about your life unvaccinated?
Getting vaccinated may carry some tiny risk, but refusing to be vaccinated carries a greater risk. The problem with a lot of anti-vaxx thinking is a narrow focus on potential vaccine risks while ignoring the reason you would take a vaccine in the first place.
With a virus that has killed something like 600,000 Americans and has caused medium-term neurologic problems, clotting disorders and possibly long-term organ damage in many others, it’s crystal-clear that at this time COVID vaccination risk is less than COVID disease risk. It’s safer to be vaccinated than to refuse.
The other very good news is that we have multiple vaccines to choose from (in the US and worldwide). At this time, it’s possible that one or more COVID vaccines will turn out to be slightly more or less risky than the others. I expect our usage to follow the data on an ongoing basis.
What happens now?
Experts are now grappling with what to do with new information about blood clots. They may determine that the J&J vaccine is not linked to the rare clotting disorder. If you look at a group of almost seven million people, you can find all kinds of spurious connections.
Or, they may determine that a connection is possible or likely. In that case, they will try to figure out if certain classes of people (say, younger than age 50) are more vulnerable to the clotting disorder than others. Then they’ll mitigate the risk by recommending that people in that class receive a different vaccine. Whether or not they’re able to identify any predisposing factors, experts can already make recommendations about what to watch for and how doctors should treat the rare effect in order to minimize the consequences to people’s health.
Finally, it’s possible that they will decide to extend the pause until they have enough information to make a better decision about which vaccines we should be giving to which people. Remember, each vaccine has a unique profile of risks and benefits. The Johnson & Johnson vaccine has been proven effective with just a single dose—a big advantage in some situations—so it will not be thrown away lightly.
Have you been vaccinated yet? If you live in California and are age 16 or older, you’re eligible now!
Visit https://myturn.ca.gov/ to find appointments for a FREE vaccine near you.
Amy Rogers, MD, PhD, is a Harvard-educated scientist, novelist, journalist, and educator. Learn more about Amy’s science thriller novels, or download a free ebook on the scientific backstory of SARS-CoV-2 and emerging infections, at AmyRogers.com.