There won’t be a cure: Why are viral infections so hard to treat?
Why are viral infections so hard to treat?
In today’s post I’d like to explain some of the basic biology of viruses. This will help you understand a future post about how this pandemic will end.
An article that circulated on Facebook last week made a rather odd argument that coronavirus is a zombie-like thing that flips back and forth between being alive and dead. The article implied that this is what makes SARS-CoV-2 so dangerous. Well, not really. But there is a legitimate point here: Are viruses really alive?
That depends on your definition of “life.” Viruses are a minimalist form of life. Imagine if Marie Kondo took a living cell and decluttered it of everything that was not absolutely essential—and then threw away a few necessary things that you can borrow instead of owning. You would get a virus. Single-celled life, such as bacteria, can do all kinds of things. They can eat, travel, defend themselves, communicate with other cells, produce waste, pass on information to their children, and they can make copies of themselves (reproduce).
Viruses, on the other hand, are much smaller than cells. They are not cells. A virus is a tiny package of information (either RNA or DNA) wrapped inside a protective shell (a protein coat). A virus cannot eat, cannot move under its own power, does not produce waste, and is unable to reproduce on its own. Thinking like a science fiction writer, I imagine a virus as a small golden chest buried in the desert by an advanced, alien civilization. Inside the chest are blueprints for a doomsday device. Human explorers encounter the chest, open it, build the device, and blow themselves up. In the final scene of this little tale, another small golden chest drifts through space in search of a new planet to infect.
In a similar way, a virus is impotent until it encounters a living cell. When they come together, the virus inserts its information (RNA or DNA) into the cell and forces the cell to build a doomsday device (more viruses). The virus hijacks the machinery of the cell in order to reproduce itself according to the instructions coded in its own RNA or DNA. Eventually the cell either bursts or dies of exhaustion, releasing many new viruses to infect more cells.
This peculiar way of life is the reason why we have very few chemical treatments (drugs) against viral infections. The first really good drug to treat infectious diseases was penicillin. Penicillin works against some classes of bacteria. It is an antibiotic, not an antiviral. Neither penicillin nor any other newer antibiotic can kill a virus or treat a viral infection. Why?
It’s pretty simple. The cells of bacteria are fundamentally different from human cells in a couple of ways. Those differences provide targets for chemical poisons that harm the bacteria, but don’t affect the cells of the human patient taking the drug. To illustrate, imagine if a poison could kill cells that contain chlorophyll (the photosynthesis chemical that makes plants green). A human could take this poison and be just fine. Same with antibiotics. They are poisons for bacteria but not for people because the bacteria possess some target molecule that we don’t.
In contrast, viruses present very few potential targets to distinguish them from humans. Seems counterintuitive, right? Viruses are more different from us than bacteria are, yet they have fewer unique features that we can target with drugs.
The answer to this riddle is in the life cycle I just described. Viruses have been thoroughly decluttered. Instead of having their own unique enzymes and systems and structures for metabolism and reproduction (like bacteria do), viruses use ours. We cannot design a drug to inhibit food consumption by viruses because they make our cells digest food for them. We cannot design a drug to block the assembly of viral proteins because our cells are doing the assembly for them.
Antiviral weapons are rare and difficult to invent because viruses use human shields.
In recent decades, a few good antiviral drugs have come into use against HIV, hepatitis and herpesviruses, and modestly effective drugs against influenza. But these drugs are not as powerful or broadly useful as most antibiotics are.
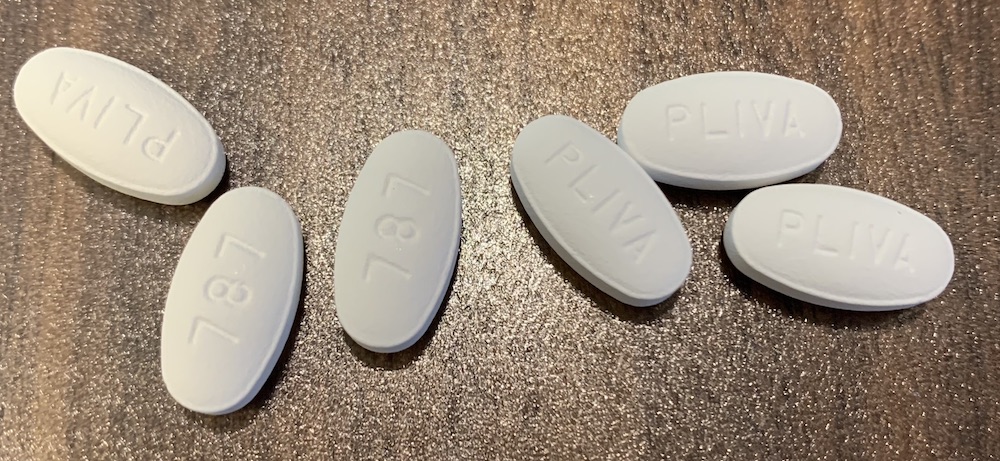
For these reasons, the end of the COVID-19 pandemic is unlikely to come from a cure. By and large, we haven’t figured out how to cure viral infections in general. We may stumble upon some already-existing pharmaceuticals (such as the much-touted chloroquine) that help the immune system fight off the coronavirus. This could increase patient survival, but would not fundamentally change the course of the pandemic.
The coronavirus pandemic will end with herd immunity, not with a cure. We will acquire that immunity either the hard way or through vaccination. I’ll discuss this in detail in a few days.
Learn more about Amy Rogers and her books, including a free ebook on the scientific backstory of SARS-CoV-2 and emerging infections, at AmyRogers.com.
 Do you like my science journalism? Read Science in the Neighborhood and learn, where does my tap water come from? How are mosquitoes managed? What happens after I flush? Where does my electricity come from?
Do you like my science journalism? Read Science in the Neighborhood and learn, where does my tap water come from? How are mosquitoes managed? What happens after I flush? Where does my electricity come from?
0 Comments
Share this:
0 Comments